Understanding Emotional Trauma and Healing Pathways
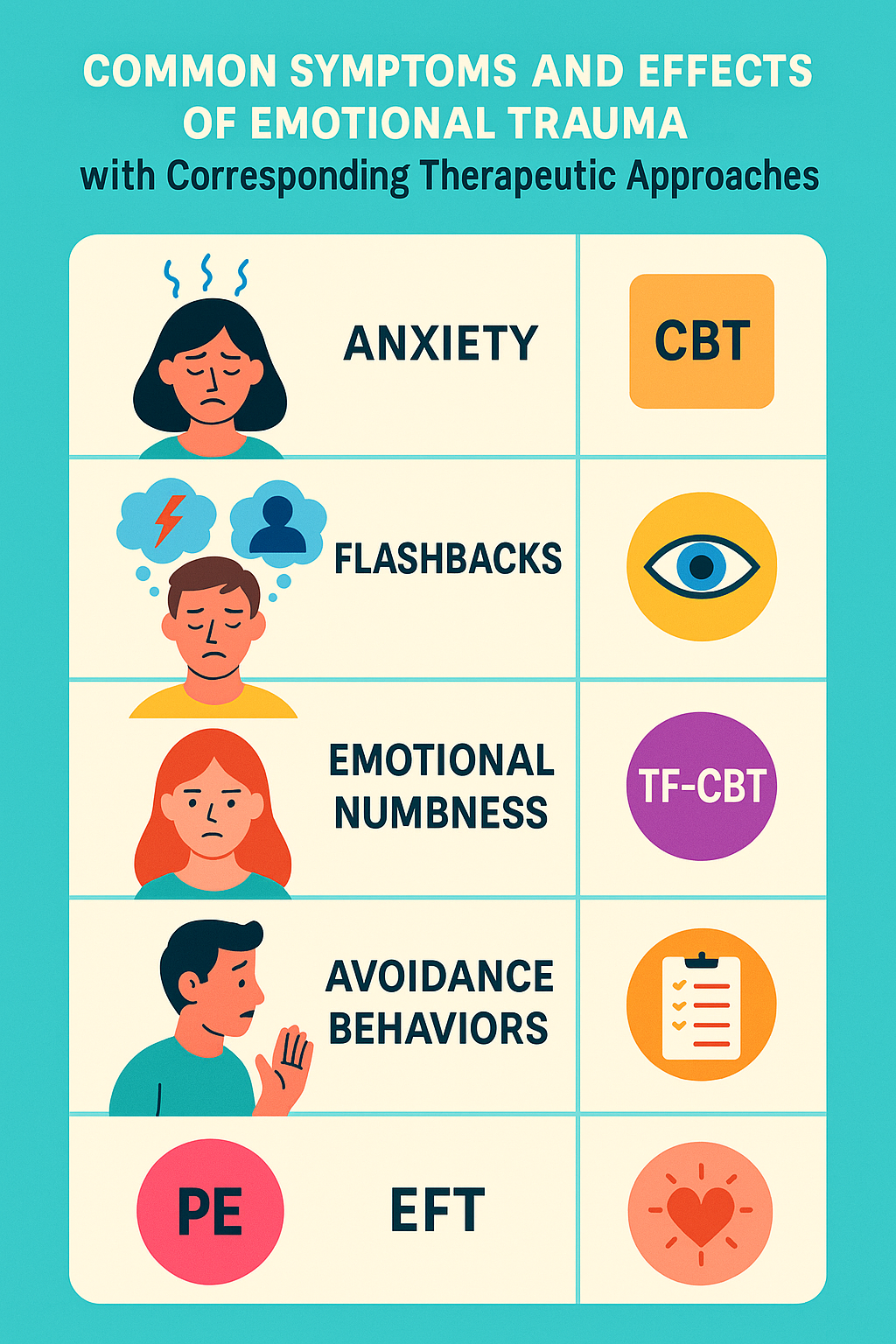
Therapy for emotional trauma is a specialized approach to helping individuals heal from distressing experiences that have deeply impacted their mental health and wellbeing. If you’re searching for ways to address emotional trauma, here are the five most effective therapeutic approaches:
- Cognitive Behavioral Therapy (CBT) – Helps restructure negative thought patterns
- Eye Movement Desensitization and Reprocessing (EMDR) – Processes traumatic memories through bilateral stimulation
- Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) – Specialized for children and adolescents
- Prolonged Exposure Therapy (PE) – Gradually confronts trauma memories to reduce avoidance
- Emotionally-Focused Therapy (EFT) – Addresses trauma through emotional connection and attachment
Emotional trauma can result from a wide range of experiences – from one-time events like accidents or assaults to ongoing situations such as abuse or neglect. Over 50% of people experience at least one traumatic event in their lives, with 3.6% of US adults experiencing PTSD in the past year alone.
Your responses to trauma are normal reactions to abnormal events.
Trauma affects not just your thoughts but your entire being – your emotions, your body, and your relationships. When traumatic experiences overwhelm your natural coping mechanisms, they can leave lasting imprints that disrupt daily functioning.
The good news? Healing is possible. With appropriate support and evidence-based therapeutic approaches, you can process these experiences and reclaim your sense of safety and wellbeing.
I’m Emmanuel Romero, a Licensed Marriage & Family Therapist specializing in therapy for emotional trauma with over seven years of experience helping individuals steer their healing journeys through evidence-based trauma treatment approaches. My work as a Mental Health Specialist and private practice owner has given me experience in supporting clients through various trauma-informed therapeutic modalities.
1. Cognitive Behavioral Therapy (CBT) for Trauma
When it comes to healing from emotional wounds, Cognitive Behavioral Therapy (CBT) stands as one of our most trusted allies. This approach isn’t just well-researched—it’s proven to help people reclaim their lives after trauma. CBT works by exploring the powerful connection between your thoughts, feelings, and behaviors, gently helping you identify and reshape the negative thought patterns that may have developed after difficult experiences.

In our San Clemente practice, we often talk about “trauma lenses”—those distorted ways of seeing yourself and the world that can form after traumatic events. You might find yourself thinking thoughts like “I’ll never feel safe again” or “I’m broken beyond repair.” These thoughts feel absolutely real when you’re wearing those lenses, but CBT offers a way to gently remove them and see things from a fresher, more balanced perspective.
Research consistently backs up what we see in our practice. According to the National Institute of Mental Health, CBT approaches show remarkable effectiveness for trauma recovery, with many people experiencing significant relief from their symptoms.
How CBT Provides Therapy for Emotional Trauma
Therapy for emotional trauma using CBT isn’t about erasing what happened—it’s about changing your relationship with those experiences. Here’s how it works:
First, we focus on cognitive restructuring—a fancy term for identifying and gently challenging unhelpful thought patterns. For example, if you survived a car accident, you might believe “I can never be safe in a vehicle again.” Through thoughtful conversation and careful evidence-gathering, we help you develop more balanced perspectives like “While driving carries some risks, I can take precautions to increase my safety.”
Many trauma survivors develop avoidance as a primary coping strategy. While this offers temporary relief, it often reinforces fear in the long run. CBT helps you gradually face trauma-related memories and situations in a controlled, supportive environment—at your pace, never pushing faster than feels manageable.
One client recently shared with me: “I was convinced that avoiding all reminders of what happened was my only option. Through our CBT work, I learned that carefully facing these memories—though incredibly difficult—actually reduced their grip on me. They didn’t disappear, but they no longer run my life.”
Beyond changing thought patterns, CBT equips you with practical coping strategies for managing trauma symptoms in daily life. These include grounding techniques for flashbacks, breathing exercises for anxiety, improved sleep habits, and activities that help lift depression.
What makes CBT particularly valuable is its lasting impact. The skills you learn become part of your personal toolkit, helping you manage not just current symptoms but also potential future triggers. Studies show that 50-60% of people who complete CBT for PTSD experience significant symptom reduction, with many no longer meeting diagnostic criteria for PTSD after treatment.
At Mr. Therapist, we’ve seen how CBT can transform lives after trauma. While the journey isn’t always easy, having these evidence-based tools on your side makes healing not just possible, but probable.
2. Eye Movement Desensitization and Reprocessing (EMDR)
EMDR therapy stands as a approach to trauma healing that has transformed millions of lives worldwide. When Dr. Francine Shapiro first developed this method in 1987, few could have predicted how it would change the landscape of therapy for emotional trauma. This unique approach uses bilateral stimulation—typically through guided eye movements—to help the brain process traumatic memories that have become “stuck” in your nervous system.

At its core, EMDR works on the Adaptive Information Processing model. This theory suggests that trauma essentially disrupts your brain’s natural healing ability. Think of it like this: when you cut your finger, your body naturally knows how to heal the wound. Similarly, your brain has natural mechanisms to process difficult experiences—but trauma can overwhelm these systems. When traumatic memories remain unprocessed, they continue to feel fresh and raw when triggered, making you feel as if the event is happening right now rather than in the past.
In our practice at Mr. Therapist, we’ve witnessed truly remarkable changes through EMDR. I remember one client who beautifully described her experience: “Before EMDR, remembering my assault felt like reliving it—the same terror, the same helplessness flooded through me. After treatment, I can recall what happened without being overwhelmed. It feels like a memory from the past, not a current threat.”
Benefits of EMDR in Therapy for Emotional Trauma
What makes EMDR particularly special as a form of therapy for emotional trauma are several unique benefits that set it apart from traditional approaches.
Minimal verbal recounting provides immense relief for many trauma survivors. Unlike some traditional therapies that require you to tell your story in detail, EMDR doesn’t demand extensive storytelling. This makes it particularly valuable if you find it overwhelming to talk about your trauma or if you experienced trauma before you had the words to describe it (pre-verbal trauma).
The potential for rapid relief often surprises both clients and clinicians alike. While everyone’s healing journey is unique, EMDR can sometimes work more quickly than traditional talk therapies. Research paints an encouraging picture: 84-90% of single-trauma survivors no longer meet criteria for PTSD after just three 90-minute sessions. For those with multiple traumas, significant improvement typically occurs within 6-12 sessions.
EMDR’s physiological approach sets it apart from purely cognitive therapies. It works directly with how trauma is stored in both your brain and body. The bilateral stimulation—whether through eye movements, gentle taps, or alternating tones—appears to stimulate your brain’s information processing system in ways similar to REM sleep. This allows traumatic memories to be processed and integrated into your broader life narrative.
The evidence supporting EMDR is substantial. A comprehensive 2014 review of 24 studies suggested that EMDR can work more efficiently than trauma-focused CBT. The American Psychological Association has recognized it as an effective treatment for PTSD, and both the Department of Veterans Affairs and Department of Defense list EMDR as a ‘best practice’ for treating veterans with PTSD.
One of the most powerful aspects of EMDR is how it helps transform negative beliefs that formed during trauma. For instance, a client who survived a serious accident initially believed “I am helpless.” Through EMDR reprocessing, this shifted to “I am resourceful and can handle difficult situations.”
As Dr. Shapiro herself explains: “Processing does not mean talking about it. Processing means setting up a learning state that will allow experiences that are causing problems to be ‘digested’ and stored appropriately in your brain.”
For more detailed information about this approach, the EMDR International Association offers comprehensive resources about the therapy’s protocols and applications.
3. Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) for Youth
When children experience trauma, they need an approach specifically designed for their developmental stage and unique needs. Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) is exactly that—a specialized treatment approach created with young people in mind. This evidence-based therapy beautifully weaves together elements from cognitive-behavioral, attachment, family, and humanistic approaches to help children and teens heal.

In my work at Mr. Therapist, I’ve seen how differently children process trauma compared to adults. Many young clients walk through our doors unable to articulate what they’re feeling. Instead, their trauma shows up as behavioral challenges, falling grades, or difficulties with friends and family. Rather than clearly saying “I’m experiencing flashbacks,” a child might have tantrums, become withdrawn, or struggle to focus in school.
TF-CBT offers these young people a path to healing that honors their developmental needs while providing structure and support. What makes this approach particularly powerful is that it doesn’t just focus on the child—it brings caregivers into the healing journey too.
How TF-CBT Addresses Emotional Trauma in Youth
Therapy for emotional trauma with TF-CBT follows a thoughtful, step-by-step approach that practitioners remember using the acronym PRACTICE:
We begin with psychoeducation and parenting skills. I love watching the relief on parents’ faces when they understand that their child’s behaviors aren’t “bad behavior” but normal responses to abnormal events. During this phase, families learn about trauma’s effects and caregivers develop skills to support their child’s healing.
“I thought my son was just being defiant,” one mother told me. “Learning that his anger outbursts were actually trauma responses completely changed how I responded to him. Instead of punishment, I could offer understanding.”
Next, we teach relaxation techniques that help children manage the physical symptoms of trauma—racing heart, tight muscles, trouble sleeping. Children often enjoy learning these skills, which give them a sense of control over their bodies’ reactions.
The affective expression and regulation component helps young people recognize and name their feelings—something many traumatized children struggle with. We might use art, play, or other age-appropriate activities to help them connect with emotions they’ve learned to suppress.
Through cognitive coping and processing, children begin to understand how thoughts affect feelings and behaviors. We gently help them identify and challenge unhelpful thoughts that developed after their trauma.
Perhaps the most transformative element is creating a trauma narrative—a gradual, supported process of telling their story. I remember a 10-year-old client who initially couldn’t speak about her experience but eventually created a picture book about a brave lioness who survived danger. This symbolic storytelling helped her process what happened without being overwhelmed.
When appropriate, we incorporate in vivo exposure, helping children face trauma reminders safely to overcome avoidance. This might look like a child who was in a car accident gradually becoming comfortable riding in vehicles again.
Conjoint sessions bring children and caregivers together, allowing young people to share their trauma narratives with supportive adults who have been prepared to respond with empathy and understanding.
Finally, we focus on enhancing safety and future development—building skills for personal protection and healthy growth moving forward.
TF-CBT typically spans 12-20 sessions and has impressive results. Research from the Trauma-Focused Cognitive Behavioral Therapy program shows significant reductions in PTSD symptoms, depression, anxiety, and behavioral problems.
What truly sets TF-CBT apart is its family approach. By equipping parents and caregivers with understanding and skills, the therapy creates a supportive home environment where healing continues long after formal sessions end. This builds resilience not just in the child but throughout the family system.
As one father shared after his family completed TF-CBT: “Before, I felt helpless watching my daughter suffer. Now we have a shared language about trauma and healing. Her nightmares haven’t completely stopped, but when they happen, she knows I understand, and we have tools to use together. We’re healing as a family.”
4. Prolonged Exposure Therapy (PE) for Trauma Survivors
Prolonged Exposure Therapy (PE) stands as one of the most powerful tools we have for healing trauma. Developed by Dr. Edna Foa, this approach tackles what many trauma survivors know all too well—the instinct to avoid anything that reminds us of what happened.

Here at Mr. Therapist, we see it all the time. After something traumatic happens, avoiding reminders feels like the only way to cope. It makes perfect sense—why would anyone want to revisit their most painful experiences? But over time, this avoidance can actually keep wounds from healing, shrinking your world smaller and smaller as you work to stay away from people, places, or situations that might trigger difficult memories.
PE offers a different path. By carefully, gradually facing what you’ve been avoiding—with support every step of the way—you can finally process what happened and reclaim the parts of life you may have lost.
The Efficacy of PE in Healing Emotional Trauma
Therapy for emotional trauma using PE isn’t about diving into the deep end right away. Instead, we take a thoughtful, step-by-step approach that typically includes:
Education first. We start by helping you understand how trauma affects the mind and body, and why—even though it feels counterintuitive—facing your memories can actually help them lose their power over you.
Simple breathing techniques become your anchor. These practical skills help manage anxiety when memories feel overwhelming, giving you a sense of control throughout the process.
Imaginal exposure involves recounting your traumatic experience during sessions in a safe space. Many clients record these narratives and listen to them between sessions. One client described this process like “watching a movie that used to be terrifying slowly become just another film.”
In vivo exposure means gradually approaching real-life situations you’ve been avoiding. For someone who survived a car accident, this might mean sitting in a parked car, then eventually becoming comfortable as a passenger, and finally returning to driving.
PE typically unfolds over 8 to 15 sessions of 90 minutes each, though we always tailor the pace to what feels manageable for you.
The research behind PE is remarkably strong. Studies consistently show about 80% of people who complete the treatment experience significant relief from their PTSD symptoms. Many no longer meet the criteria for PTSD diagnosis at all by the end of treatment.
I remember working with Terry (name changed), a 42-year-old earthquake survivor who came to us unable to even look at tall buildings without panic attacks. “At first, I couldn’t even look at tall buildings without panicking,” she shared. “Through PE, I gradually confronted these fears—first in my imagination, then in real life. Each exposure was challenging, but my anxiety decreased more quickly than I expected. Now I can go anywhere in the city without that constant fear.”
I won’t sugarcoat it—PE requires courage. There will be moments of discomfort as you face what you’ve been avoiding. But this discomfort is temporary and manageable, especially with support. And on the other side lies freedom that many clients didn’t believe was possible.
As Dr. Foa herself explains: “PE helps patients emotionally process their traumatic experiences by having them repeatedly approach trauma-related thoughts, feelings, and situations that they have been avoiding due to the distress they cause. Through repeated exposure exercises, patients learn that trauma-related memories and cues are not dangerous and do not need to be avoided.”
When you’re ready to break free from the grip of traumatic memories, PE offers a proven path forward—one step at a time, always at your pace, and never alone.
5. Self-Care Strategies for Healing Emotional Trauma
The journey of healing from emotional trauma doesn’t just happen in the therapist’s office – it continues in your daily life through intentional self-care practices. These practices aren’t luxuries or indulgences; they’re essential components of the healing process that help rebuild your sense of safety, control, and wellbeing.

At Mr. Therapist, we’ve seen how powerful consistent self-care can be in supporting our clients’ healing journeys. When you’ve experienced trauma, your nervous system often remains in a heightened state of alert. Self-care practices help regulate this system, creating more moments of calm and safety.
Mindfulness practices form a cornerstone of trauma recovery. Simple activities like focused breathing, body scans, or guided meditations can help you stay grounded in the present moment rather than being pulled into traumatic memories. Even just five minutes of mindfulness daily can make a significant difference in managing trauma symptoms.
Healthy habits around sleep, nutrition, and movement provide your body and brain with the resources needed for healing. Trauma takes a physical toll, and nurturing your body creates a foundation for emotional recovery. This might look like establishing a consistent sleep schedule, adding more nutrient-rich foods to your meals, or finding forms of movement that feel good in your body.
Self-compassion exercises help counter the harsh self-judgment that often accompanies trauma. Many survivors struggle with feelings of shame or self-blame. Learning to speak to yourself with the same kindness you would offer a dear friend can gradually transform your relationship with yourself.
“I used to beat myself up constantly about what happened and how I responded,” shared one client. “Learning self-compassion felt awkward at first, but it’s been life-changing. I now understand that my reactions were normal responses to an abnormal situation.”
Here are some self-care activities our clients have found particularly helpful in their therapy for emotional trauma:
- Journaling to process emotions and track healing progress
- Spending time in nature to calm the nervous system
- Creating art or music as forms of expression
- Establishing healthy boundaries in relationships
- Practicing gentle yoga or tai chi for mind-body connection
- Using grounding techniques during flashbacks or anxiety
- Engaging in pleasurable activities that bring joy
The Role of Social Support in Recovery
While self-care includes many solo practices, connecting with others plays a crucial role in trauma healing. Humans are wired for connection, and trauma often damages our sense of safety in relationships. Rebuilding supportive connections is both challenging and healing.
Connecting with others who understand trauma can reduce the isolation many survivors feel. This doesn’t mean you need to share your story with everyone, but having even one or two people who can listen without judgment makes a tremendous difference.
Participating in support groups offers validation and perspective. Hearing others’ experiences can normalize your own reactions and provide hope as you witness others’ healing journeys. Many clients tell us that support groups help them feel less alone and offer practical coping strategies they hadn’t considered.
Fostering relationships that feel safe and supportive creates corrective experiences that counteract trauma’s message that the world is dangerous and people can’t be trusted. These connections might include friends, family members, faith communities, or activity groups centered around shared interests.
One client described her experience: “After my assault, I isolated myself completely. Part of my healing has been slowly letting people back in—first my therapist, then a support group, and eventually close friends. Each positive interaction helps rewire my brain to remember that not everyone will hurt me.”
Healing isn’t linear, and some days will be harder than others. On difficult days, even simple acts of self-care like drinking enough water or taking a shower can be meaningful victories. The key is consistency and self-compassion, celebrating small steps while being gentle with yourself when you struggle.
Through combining professional therapy for emotional trauma with intentional self-care practices and supportive relationships, you create a comprehensive approach to healing that addresses your needs as a whole person—mind, body, and spirit.
5. Self-Care Strategies for Healing Emotional Trauma
The journey of healing from emotional trauma doesn’t just happen in the therapist’s office—it unfolds in the small choices we make each day. While professional therapy for emotional trauma provides essential guidance and support, what you do between sessions can profoundly impact your recovery journey.

At Mr. Therapist, we often tell our clients that healing is like tending a garden—therapy sessions might plant the seeds, but your daily self-care practices are the sunshine and water that help those seeds grow. Let’s explore some practices that can nurture your healing process.
Your body holds the memories of trauma just as much as your mind does. That’s why movement and exercise can be so powerful—even gentle activities like a 15-minute walk or some morning stretches can help release the tension that trauma locks into your muscles and tissues. One client shared, “On days when memories feel overwhelming, I put on my shoes and just walk. Something about moving my body helps me feel more in control again.”
Mindfulness practices offer another anchor when trauma threatens to pull you into the past. Simple exercises like focusing on your breath for five minutes or noticing the sensations of warm water on your hands while washing dishes can strengthen your ability to stay present. The beauty of mindfulness is that it doesn’t require special equipment or settings—just your attention to the present moment.
Sleep often becomes a casualty of trauma, yet it’s during rest that much of our emotional processing and healing occurs. Creating a consistent sleep routine might include having a cup of caffeine-free tea before bed, dimming lights an hour before sleep, or listening to a calming meditation. These small rituals signal to your body that it’s safe to rest.
What you put into your body matters too. Nourishing food and adequate hydration provide the building blocks your brain needs to heal. This doesn’t mean perfect eating—it means being gentle with yourself while recognizing that regular meals with protein, healthy fats, and colorful vegetables help stabilize mood and energy.
Many trauma survivors find that words sometimes fail to capture their experiences. This is where creative expression shines—whether through journaling, drawing, singing, or movement. Art bypasses the logical brain and allows emotions to flow in ways that conversation sometimes can’t. One client finded that coloring mandalas during difficult moments helped her stay grounded when memories surfaced.
Nature has a remarkable way of soothing our nervous systems. Even brief moments of connection with the natural world—feeling the sun on your face, watching birds at a feeder, or tending to a small plant—can reduce stress hormones and remind us that we’re part of something larger than our trauma.
Learning to set healthy boundaries is particularly important for trauma recovery. This might mean limiting exposure to distressing news, practicing saying “no” to demands that deplete you, or creating physical spaces in your home that feel completely safe. Your healing journey deserves protection.
While substances like alcohol might temporarily numb difficult feelings, they ultimately interfere with natural healing processes. Limiting substance use allows your body and mind to process emotions more effectively, even when that processing involves discomfort.
The Role of Social Support in Recovery
Perhaps one of the deepest wounds trauma inflicts is the sense of profound isolation. As humans, we’re wired for connection, and rebuilding safe relationships forms a crucial part of healing.
Support groups offer a unique kind of healing. Sitting in a circle with others who understand your experience without explanation can dissolve shame like nothing else. As one client told me, “The first time I shared my story in group and saw nodding instead of shock or pity, something inside me relaxed that had been tense for years.”
Not everyone in your life needs to know your trauma story. Selective sharing with a few trusted individuals who have shown they can listen without judgment or trying to “fix” you creates islands of safety in your social world.
For those not ready for in-person connection or those with specialized experiences, online communities can provide understanding and validation. Many clients find comfort in knowing they can connect with others at 3 AM when nightmares disrupt sleep.
When you’re further along in your healing journey, helping others can transform your relationship with your trauma. Volunteering, mentoring, or simply supporting a friend in need can help create meaning from difficult experiences.
Healing isn’t linear—there will be days of progress and days of setbacks. What matters is the overall trajectory and the compassion you show yourself along the way. As one resilient client put it, “I’ve learned that taking care of myself isn’t selfish or indulgent—it’s the foundation that makes all other healing possible.”
Your trauma may be part of your story, but with intentional self-care and support, it doesn’t have to define your future. Each small act of self-care is an act of reclaiming your life, one moment at a time.
Finding the Right Therapist for Emotional Trauma
Finding the right therapist is perhaps one of the most important decisions you’ll make in your healing journey. The therapeutic relationship itself is a powerful healing factor, particularly for trauma survivors whose trust may have been severely damaged by past experiences.

At Mr. Therapist, we understand that seeking help for trauma can feel overwhelming and even frightening. Many of our clients share that they consulted several therapists before finding the right fit—and I want to assure you that’s completely normal and appropriate. Finding someone you connect with matters deeply in this process.
What to Look for in a Trauma Therapist
When searching for someone to provide therapy for emotional trauma, there are several key qualities to consider.
First and foremost, look for a trauma-informed approach. A good trauma therapist understands how trauma affects your brain, body, and nervous system. They create safety in therapy sessions and carefully avoid practices that might retraumatize you. They recognize that what might appear as “resistance” often represents your body’s natural survival responses.
Specific trauma training is equally important. Ask potential therapists about their specialized training in evidence-based trauma treatments like EMDR, CBT, TF-CBT, Prolonged Exposure, or Emotionally-Focused Therapy. Don’t hesitate to inquire about their experience with your specific type of trauma. A therapist who has worked extensively with similar situations will likely have valuable insights.
Your cultural background, gender identity, and personal history all influence how you experience trauma. A therapist with cultural competence will respect and understand these dimensions rather than applying a one-size-fits-all approach. This awareness creates space for all aspects of your identity in the healing process.
Consider the therapeutic style that might work best for you. Some therapists take a more directive approach, providing specific exercises and homework. Others are more client-led, following your lead in sessions. Some focus primarily on present coping strategies, while others explore past experiences in depth. Neither approach is inherently better—it’s about what feels most helpful for your unique needs.
Finally, don’t overlook practical considerations like location, cost, insurance acceptance, session format (in-person vs. virtual), and scheduling flexibility. These factors matter tremendously in creating a sustainable therapeutic relationship that can support you throughout your healing journey.
Questions to Ask Potential Therapists
When interviewing therapists for therapy for emotional trauma, consider asking these revealing questions:
“What is your experience and training in treating trauma, specifically my type of trauma?” This helps you gauge their expertise with your particular situation.
“What therapeutic approaches do you use for trauma, and why?” Their answer reveals both their knowledge base and their ability to explain their methods clearly.
“How do you create safety in therapy sessions?” Safety is fundamental to trauma work, and a good therapist should have specific practices in place.
“What role do you see me playing in my healing process?” This helps clarify expectations and ensures the therapist values your agency.
“How do you measure progress in trauma therapy?” This shows whether they have a thoughtful approach to tracking healing beyond just “feeling better.”
The Importance of Therapeutic Fit
Research consistently shows that the quality of your connection with your therapist is one of the strongest predictors of positive outcomes in therapy. This “fit” is somewhat subjective—a therapist who works wonderfully for one person might not be right for another.
Pay attention to how you feel during your initial interactions. Do you feel respected and truly heard? Does the therapist explain concepts in ways you can understand? Do they respond thoughtfully to your concerns? While therapy sometimes involves discomfort as you address difficult experiences, you should generally feel safe and supported by your therapist.
One of our clients beautifully described her search for the right therapist: “I saw three different therapists before finding the right fit. With the first two, something felt off, though I couldn’t exactly explain what. When I met my current therapist, I just knew—there was a sense of being truly seen and understood. That connection has made all the difference in my healing.”
At Mr. Therapist, we offer a complimentary 15-minute consultation to help determine if our approach aligns with your needs. We believe that finding the right therapeutic match is crucial for effective trauma work.
You are hiring a therapist to provide a service, and you have every right to seek someone who meets your specific needs. The effort invested in finding the right therapist pays tremendous dividends in your healing journey.
You can learn more about our trauma-informed approach through Emotionally Focused Individual Therapy, which many clients find particularly helpful for processing emotional trauma.
Frequently Asked Questions about Therapy for Emotional Trauma
How do I know if I need professional therapy for emotional trauma?
Recognizing when to seek help for trauma isn’t always straightforward. Many of us tend to minimize our experiences, thinking “it wasn’t that bad” or “others have it worse.” But trauma isn’t measured by comparing your experience to someone else’s—it’s about how an event has affected you.
Your body and mind will often send signals when traumatic experiences need professional attention. You might notice persistent nightmares or flashbacks that don’t seem to fade with time. Perhaps anxiety or depression has settled in like an unwelcome houseguest who refuses to leave. When these symptoms linger for more than a month and start interfering with your daily life—making it difficult to work, maintain relationships, or simply feel like yourself—it’s usually time to reach out.
I’ve had many clients tell me they delayed seeking therapy for emotional trauma because they were using alcohol, food, or overworking to manage their symptoms. While these coping mechanisms might provide temporary relief, they often create additional problems without addressing the underlying trauma.
One client shared with me: “I kept telling myself I should just ‘get over it.’ Seeking therapy was the best decision I made. My therapist helped me understand that trauma isn’t a competition, and my suffering was real and deserved attention.”
If you’re experiencing dissociation—feeling disconnected from yourself or your surroundings—or having thoughts of harming yourself, please don’t wait. These are important signals that professional support would be beneficial. Seeking help isn’t a sign of weakness—it’s an act of courage and self-care.
Can medication assist in therapy for emotional trauma?
Medication can indeed play a supportive role in trauma recovery, particularly when symptoms are severe enough to interfere with daily functioning or make it difficult to engage in therapy effectively.
For many trauma survivors, the brain’s alarm system gets stuck in “on” mode, creating overwhelming anxiety, intrusive thoughts, or debilitating depression. Medications like SSRIs (including sertraline/Zoloft and paroxetine/Paxil) can help regulate these neurobiological responses, creating a more stable foundation for healing work. For those experiencing trauma-related nightmares, medications like prazosin might provide relief and improve sleep quality.
That said, medication typically addresses symptoms rather than processing the trauma itself. Think of it like reducing a fever—it helps you feel better and function, but doesn’t cure the underlying infection. This is why the American Psychological Association recommends trauma-focused psychotherapy as the primary treatment, with medication as a helpful addition when needed.
At Mr. Therapist, we often collaborate with psychiatrists or primary care physicians when medication might benefit a client’s recovery. We take a holistic view of healing that respects both psychological and physiological aspects of trauma.
One client beautifully summarized her experience: “Therapy for emotional trauma gave me tools to process what happened to me, while medication helped reduce my symptoms enough that I could actually use those tools. For me, both were necessary parts of healing.”
If you’re considering medication, a thoughtful conversation with a psychiatrist or physician who understands trauma can help you weigh the potential benefits against possible side effects for your specific situation.
What coping strategies can help manage trauma-related symptoms?
While professional treatment is often essential for healing trauma, having practical tools to manage symptoms in your daily life can be incredibly empowering. Think of these strategies as first-aid techniques—they won’t heal the wound completely, but they can help you function and reduce suffering while deeper healing occurs.
Grounding techniques are particularly helpful when you’re experiencing flashbacks or dissociation. These experiences happen when your brain temporarily loses track of the present moment and gets pulled back into the trauma. Grounding helps reorient you to the here and now.
The 5-4-3-2-1 technique is one of my clients’ favorites: Name 5 things you can see, 4 things you can physically feel, 3 things you can hear, 2 things you can smell (or like to smell), and 1 thing you can taste. This simple exercise engages all your senses in the present moment, helping your brain recognize you’re safe now.
Breathing exercises can quickly calm your nervous system when anxiety spikes. Box breathing is particularly effective—inhale for 4 counts, hold for 4, exhale for 4, hold for 4, and repeat. The rhythm and focus help interrupt the panic cycle and reduce stress hormones in your body.
Many trauma survivors find journaling helpful, but with an important caveat: focus on present coping rather than detailed recounting of traumatic events (which is generally best done with therapeutic support). You might try gratitude journaling to balance trauma’s negative focus, or “containment” journaling—writing about difficult thoughts or feelings, then symbolically “containing” them by closing the journal until you’re ready to address them, perhaps in therapy.
Sleep difficulties are common with trauma, yet quality rest is crucial for healing. Creating a consistent sleep routine, limiting screen time before bed, and using relaxation techniques like progressive muscle relaxation can help create conditions for better sleep.
As one client shared: “My therapist taught me that I don’t have to be at the mercy of my trauma symptoms. These techniques don’t make the trauma disappear, but they give me ways to manage the waves when they come, which has been incredibly empowering.”
While these strategies can help manage symptoms, they work best alongside professional therapy for emotional trauma when dealing with significant trauma. You deserve comprehensive support on your healing journey.
Conclusion
The journey of healing from emotional trauma is deeply personal and often challenging, but recovery is possible. As we’ve explored throughout this article, evidence-based therapy for emotional trauma offers pathways to processing difficult experiences and reclaiming your sense of safety, connection, and joy.
Whether through Cognitive Behavioral Therapy, EMDR, Trauma-Focused CBT, Prolonged Exposure, or Emotionally-Focused Therapy, healing happens when traumatic experiences are processed in a safe, supportive environment with appropriate guidance.
“There’s hope for healing.”
This simple truth has guided countless trauma survivors forward when the path seemed darkest. At Mr. Therapist, we’ve witnessed remarkable changes as individuals rebuild their relationship with trauma—not by erasing these experiences (which isn’t possible or necessary), but by integrating them in ways that allow for post-traumatic growth and renewed engagement with life.
I remember a client who shared, “My trauma will always be part of my story, but therapy helped me ensure it’s not the whole story. I’ve reclaimed authorship of my life narrative.” Her words capture the essence of trauma recovery—not forgetting, but finding a new way forward.
If you’re struggling with the effects of emotional trauma, please be gentle with yourself. The symptoms you’re experiencing are normal reactions to abnormal events, not signs of weakness or failure. Your body and mind are doing exactly what they were designed to do in response to overwhelming experiences.
Reaching out for support is an act of courage, not weakness. Professional help can make a significant difference in your healing journey, providing both tools and understanding that friends and family—however well-intentioned—may not be equipped to offer.
Healing isn’t linear. Some days will feel like two steps forward, others like one step back. This natural ebb and flow doesn’t mean you’re failing—it’s simply part of the process. Each small victory deserves celebration, whether it’s a night without nightmares, a moment of feeling safe in your body, or simply showing up for your therapy appointment on a difficult day.
At Mr. Therapist in San Clemente, California, Manny Romero and our team specialize in trauma-informed care that honors your unique experience and resilience. We understand that trauma affects every aspect of a person—mind, body, emotions, and relationships—and our approach reflects this holistic understanding. We offer both in-person and virtual sessions to accommodate your needs and preferences.
The path forward may not always be clear or easy, but you don’t have to walk it alone. When you’re ready to take the next step in your healing journey, we’re here to walk alongside you with expertise, compassion, and unwavering support.